The Best Text Blaze Snippets (Dot Phrases) for Medical Professionals
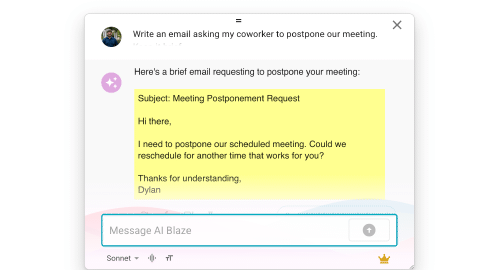
Medical professionals like doctors and nurses use dot phrases, or snippets, to increase their efficiency and accuracy, allowing them to spend more time with their patients. This collection makes it easy to start saving time with Text Blaze.
Copy templates to use them anywhere:
On this page, you’ll find a collection of dot phrase templates (or “snippets”) that health professionals can use to automate reports, prescriptions, and repetitive typing.
These snippets will drastically cut down on the time and effort you spend on administrative work, so you can spend more time doing what you do best—caring for your patients.
Patient Visits and Evaluation
Here you'll find snippets, or dot phrase templates, for items like regular visits or a history of present illness (HPI).
Use these to be more efficient with your time, creating notes in the EMR of your choice easily. Text Blaze helps resolve the pain of repetitively creating comprehensive notes, and lets you focus on your patients first.
Universal HPI Note
This snippet was created by Text Blaze Community member Timothy_Wong.
New OB Patient Intake
While this snippet is specifically for an OB, it is easily customized to any specific medical profession. Simply Click the "Copy to Text Blaze" button to add it to your account, then make the changes you need.
This snippet uses the formparagraph command, the formmenu command, and the formtext command.
Patient is {formtoggle: name=sure lmp; default=yes}sure of her LMP{endformtoggle}{formtoggle: name=unsure of lmp; default=no}unsure of her lmp{endformtoggle} LMP {note}{formdate: MM/DD/YYYY; name=date}{formtext: name=shifting; default=}{endnote: trim=right} EDD: {time: MM/DD/YYYY; at={=date}; pattern=MM/DD/YYYY; shift={=shifting}280D}
{formtoggle: name=multigravid; default=yes}Patient has a previous pregnancy history that is {endformtoggle}{formtoggle: name=uncomplicated; default=yes}uncomplicated. {endformtoggle}{formtoggle: name=complicated; default=no}complicated by {formparagraph: name=complications} {endformtoggle}.
Past medical history and past surgical history is reviewed. {formtoggle: name=significant for\ ; default=no}It is significant for {formparagraph: name=significant history}.{endformtoggle}
{formtoggle: name=transfer ob care; default=no}The patient transferred care from {formtext: name=previous doctor}. They report they have had {formmenu: default=prenatal labs; 1st trimester ultrasound\ ; 2nd trimester ultrasound; referral to MFM; oral glucose tolerance test; name=pregnancy care items; multiple=yes}. {formtoggle: name=records received; default=no}Records have been requested and received.{endformtoggle}{endformtoggle}
Family History of Colon Cancer
The following snippet makes it possible to generate a detailed report of the patient’s family history of colon cancer.
This snippet uses the Form Text command and drop-down menus.
General Notes from a Medical Assessment
This snippet will take notes for a healthcare profession completing a full medical assessment. The output will be a well-formatted summary of notes reflective of the information entered into the snippet. Some statements are generated automatically based on the age and/or sex entered, where others only display when checking a box. Many are dependent on a conditional combination of age, sex, and noted concern. Tests, screenings, and referrals can be selected at the end of the snippet.
{note: trim=yes}Please enter the following information about the patient:
Age (number of years): {formtext: name=Age}
Sex: {formmenu: default=; female; male; name=sex}
{endnote: trim=left}
- The patient is a {=Age} year old {=sex}.
- The patient's chart was reviewed and reconciled as noted in the HPI
- The patient's lifestyle was reviewed for possible impacts on health. I identified and addressed any barriers to improved health, such as age, gender, ethnic background, and, racial identity. Status of advanced health care planning was reviewed.
- The patient's self-reported or lab-reported vital signs were reviewed.
- Information was provided regarding healthy lifestyle choices and vaccinations.
- Based on recommendations for all or almost all adults, the patient was:
- Screened for depression, unhealthy alcohol use, smoking, and unhealthy drug use
- Screened for hypertension or recommended to screen for hypertension
- Offered screening for Hepatitis C and HIV
- Counseled regarding advanced care planning, including advanced directives, and offered follow up for future discussion if desired.
Specific concerns for this patient, if any:
{formtoggle: name=BMI over 25; default=no; trim=right}- BMI between 25 and 30: The patient was offered screening for diabetes. The patient given information on healthy diet and exercise for prevention of diabetes.{endformtoggle: trim=left}
{formtoggle: name=BMI over 30; default=no; trim=right}- BMI over 30: The patient was offered screening for diabetes. The patient was given information on healthy diet and exercise for weight loss and reduction of risk of diabetes and cardiac disease. {endformtoggle: trim=left}
{formtoggle: name=Having more than 1 partner in 12 months; default=no; trim=right}{endformtoggle: trim=left}
{formtoggle: name=Requesting testing for sexually transmitted infections; default=no; trim=right}{endformtoggle: trim=left}
{if: `Having more than 1 partner in 12 months` OR `Requesting testing for sexually transmitted infections`="Yes"; trim=yes}- Increased risk of sexually transmitted infection or request for testing: The patient was counseled regarding safe sexual practices and was offered laboratory testing for sexually transmitted infection, including Hepatitis B, Hepatitis C, HIV, Syphilis, gonorrhea, and chlamydia.{endif: trim=left}
{formtoggle: name=Sexually active; default=no; trim=right}{endformtoggle: trim=yes}
{if: `Sexually active`="Yes" AND sex="female" AND (age >=18 AND age <=24); trim=right}If sexually active female age 18-24, the patient was offered testing for gonorrhea and chlamydia.{endif: trim=left}
{formtoggle: name=Specific risk of HIV; default=no; trim=right}- Specific risk of HIV: The patient was advised to make a follow up appointment for discussion of pre-exposure prophylaxis for prevention of HIV.{endformtoggle: trim=left}
{formtoggle: name=Increased risk of Tuberculosis; default=no; trim=right}- Increased risk of Tuberculosis: The patient was encouraged to have Quantiferon Gold TB testing. If patient desired, an order was placed or Quantiferon Gold TB testing.{endformtoggle: trim=left}
{formtoggle: name=Tobacco/Nicotine use now or in the past; default=no; trim=right}- The patient reports {formtext: name=packyears} pack years of tobacco use{endformtoggle: trim=left}{note: trim=right}{if: `Tobacco/Nicotine use now or in the past`="Yes"; trim=left}
When was the tobacco/nicotine use?{formmenu: default=; now; quit less than 15 years ago; quit more than 15 years ago; name=tobacco; trim=right}{endif: trim=right}{endnote: trim=yes}
{if: tobacco="now"; trim=left}
- Current smoker: The patient was counseled on smoking/vaping cessation and methods to improve success with cessation.{endif: trim=left}
{if: (age >=50 AND age<=80) AND (tobacco="now" OR tobacco="quit less than 15 years ago") AND packyears>=20; trim=left}
- Increased risk of lung cancer: The patient was offered annual screening for lung cancer with low dose CT.{endif: trim=left}
{if: (age >=65 AND age <=75) AND (tobacco="now" OR tobacco="quit less than 15 years ago" OR tobacco="quit more than 15 years ago") AND sex="male"; trim=left}
- Increased risk of AAA: If lifetime cigarette use was more than 100 cigarettes, the patient was offered one-time screening ultrasound for abdominal aortic aneurysm.{endif: trim=left}
{if: (tobacco="quit less than 15 years ago" OR tobacco="quit more than 15 years ago"); trim=left}
- Patient congratulated on having quit smoking{endif: trim=left}
{formtoggle: name=Unhealthy alcohol use; default=no; trim=right}- Unhealthy alcohol use: Depending on the patient's preference, the patient was encouraged to follow up with me, was referred to counseling, or was advised to seek an alcohol counseling/treatment program.{endformtoggle: trim=left}
{formtoggle: name=Concern of depression or anxiety; default=no; trim=right}- Concern of depression or anxiety: Depending on the patient's preference, the patient was encouraged to follow up with me or was referred to counseling.{endformtoggle: trim=left}
{formtoggle: name=Elevated blood pressure; default=no; trim=right}- Elevated blood pressure: the patient was encouraged to follow up with me.{endformtoggle: trim=left}
{formtoggle: name=Female with personal or family history of BRCA related cancer or of Ashkenazi Jewish Ancestry; default=no; trim=right}{endformtoggle: trim=left}
{if: `Female with personal or family history of BRCA related cancer or of Ashkenazi Jewish Ancestry`="Yes" AND sex="female"; trim=yes}- Increased risk of breast cancer: The patient was offered BRCA testing{endif: trim=left}
{formtoggle: name=History of diabetes, hypertension, or tobacco use; default=no; trim=right}{endformtoggle: trim=left}
{if: `History of diabetes, hypertension, or tobacco use`="Yes" AND (age >=40 AND age <=75); trim=yes}- History of diabetes, hypertension, or tobacco use: The patient was offered laboratory testing as needed and was asked to return for review of risk/benefit balance of daily aspirin or statins for the prevention of cardiovascular disease.{endif: trim=left}
{if: `History of diabetes, hypertension, or tobacco use`="Yes" AND (age<40 OR age>75); trim=yes}- History of diabetes, hypertension, or tobacco use: The patient was informed that there is no clear benefit for either aspirin or statins in their age group but that we will review recommendations for them at each annual health visit.{endif: trim=left}
{formtoggle: name=Fair skin; default=no; trim=right}- Fair skin: The patient was counseled regarding minimizing exposure to ultraviolet radiation.{endformtoggle: trim=left}
{formtoggle: name=Concern for memory loss; default=no; trim=right}- Concern for memory loss: The patient was advised to follow up for further testing or to seek in-person care. If a trusted support person was present in the visit, this person agreed to help coordinate this follow-up.{endformtoggle: trim=left}
{if: (`BMI over 25` OR `BMI over 30` OR `Having more than 1 partner in 12 months` OR `Requesting testing for sexually transmitted infections` OR `Sexually active` OR `Specific risk of HIV` OR `Increased risk of Tuberculosis` OR `Unhealthy alcohol use` OR `Concern of depression or anxiety` OR `Elevated blood pressure` OR `Female with personal or family history of BRCA related cancer or of Ashkenazi Jewish Ancestry` OR `History of diabetes, hypertension, or tobacco use` OR `Fair skin` OR `Concern for memory loss`="Yes") OR tobacco<>""; trim=right}- The patient was offered Behavioral health counseling for any specific concerns noted above{else}No specific concerns noted above.{endif: trim=left}
{note}
The following statements are generated based on age and sex entered at the top{endnote}
{if: (age>=18 AND age<=55) AND sex="female"; trim=left}
- The patient was screened for domestic violence and, if able to become pregnant, was recommended to take folic acid supplementation of at least 0.4mg daily{endif: trim=left}
{if: (age>=21 AND age<=65) AND sex="female"; trim=left}
- I reviewed that the patient's screening for cervical cancer is up to date or have referred her to OB/Gyn for this.{endif: trim=left}
{if: (age>=45 AND age<=85); trim=left}
- The patient was offered colorectal cancer screening if indicated.{endif: trim=left}
{if: age>=65 AND sex="female"; trim=left}
- The patient was offered a bone density scan for screening for osteoporosis if due.{endif: trim=left}
{if: (age>=45 AND age<=75); trim=left}
- The patient was offered screening mammogram for breast cancer if due.{endif: trim=left}
{if: age>=65; trim=left}
- The patient's fall risk was reviewed and, if elevated, multifactorial interventions, including exercise, were recommended.{endif: trim=left}
Testing or screening ordered during this visit:
{note: trim=right}{formmenu: Basic labs, including: CBC, CMP, Hemoglobin A1C, TSH, Lipids; Hepatitis B, Hepatitis C, HIV, Syphilis; Gonorrhea/chlamydia; Quantiferon Gold TB; Low dose CT screening for lung cancer; Ultrasound for AAA; BRCA testing; FIT, Cologard; Bone density scan; Mammogram; name=testing; multiple=yes}{endnote: trim=right}
{if: testing=[]}None{else}{=join(testing,", ")}{endif}
Referrals placed during this visit:
{note: trim=right}{formmenu: Behavioral Health; Gastroenterology for colonoscopy; OB/Gyn for women's health; name=referrals; multiple=yes}{endnote: trim=right}
{if: referrals=[]}None{else}{=join(referrals,", ")}{endif}
The patient was advised to follow up at least annually for preventive health care, sooner as needed for review of results or discussion of concerns raised.
The patient verbalized a clear understanding of my instructions and was agreeable with the plan.
Calculators and Assessments
This section includes a variety of snippets of calculators and assesment tools. They can be used to quickly complete calculations like BMI or run an assessment like CHA2DS2-VASc. While these snippets have been tested, always use your medical judgement when reviewing results.
BMI Calculator
This snippet can be used to determine a patient’s BMI. It uses the formtext command and formulas.
Weight {formtext: name=weight; default=150; cols=5} {formmenu: default=lbs; kgs; name=weight units} Height: {formtext: name=height; cols=3; default=70} {formmenu: default=inches; CMs; name=height units} BMI: {=BMI; format=,.2f}{note: preview=no}
Calculations {kgs=weight/2.2046 if `weight units`="lbs" else weight} {cms=height*2.54 if `height units`="inches" else height} {bmi=(kgs/cms/cms)*10000}{endnote}
Creatinine Clearance Calculator
This snippet is a dot phrase to calculate CrCl according to the Cockcroft - Gault equation.
Age (years): {formtext: name=age}
{if: `weight units`="kgs"}Weight{note} (kg){endnote}: {formtext: name=weight}{formmenu: default=lbs; kgs; name=weight units}{note} Norm: 1 - 150 kgs{endnote}{endif}{if: `weight units`="lbs"}Weight{note} (lbs){endnote}: {formtext: name=weight}{formmenu: lbs; default=kgs; name=weight units}{note} Norm: 2 - 300 lbs{endnote}{endif}
{if: `height units`="cm"}Height{note} (cm){endnote}: {formtext: name=height}{formmenu: default=inches; cm; name=height units}{note} Norm: 152 - 213 cm{endnote}{endif}{if: `height units`="inches"}Height{note} (inches){endnote}: {formtext: name=height}{formmenu: default=inches; cm; name=height units}{note} Norm: 60 - 84 inches{endnote}{endif}
Sex: {formmenu: Male; Female; name=sex}
Results Original Cockcroft and Gault formula result: {=round(originalresult)} mL/min
Crockcroft and Gault formula using Ideal Body Weight: {=round(ibwresult)} mL/min
{if: bmi<18.5}Because BMI is under 18.5, it is recommended to use the unadjusted result.{elseif: bmi<25}Because BMI is between 18.5 and 25, it is recommended to use the Ideal Body Weight result.{elseif: BMI>25}Crockcroft and Gault formula using Adjusted Body Weight: {=round(adjustedresult)} mL/min
Because BMI >25, it is recommended to use the Adjusted Body Weight result.{endif} {formtoggle: name=Show evidence and formulas} Cockcroft-Gault formula for mL/min = (140 – age) × (weight in kg) × (0.85 if female) / (72 × SCR in mg/dL)
For Ideal Body Weight calculations, the following formula is used: Males: 50+(2.3*(height in inches-60)) Females: 45.5+(2.3*(height in inches-60))
Adjusted bodyweight is calculated as Ideal Body Weight + 0.4 * (actual weight - ideal body weight)
BMI is calculated using 703*(weight in pounds/(height in inches^2)) for imperial measurements, and weight in kg/(height in meters^2) for metric.{endformtoggle}{note: preview=no}
Original research: https://pubmed.ncbi.nlm.nih.gov/1244564/, https://pubmed.ncbi.nlm.nih.gov/22576791/
**CALCULATIONS** Transforming units: {kg=weight/2.2046 if `weight units`="lbs" else weight} {inches=height if `height units`="inches" else height/2.54} {meters=height*0.0254 if `height units`="inches" else height*0.01}
Ideal body weight {maleibw=50+(2.3*(inches-60))} {femaleibw=45.5+(2.3*(inches-60))}
Adjusted body weight {maleabw=maleibw+0.4*(kg-maleibw)} {femaleabw=femaleibw+0.4*(kg-maleibw)}
BMI {bmi=kg/(meters^2)}
FOR MALE {if: sex="Male"} {originalresult=((140-age)*kg)/(72*scr)} {ibwresult=((140-age)*maleibw)/(72*scr)} {adjustedresult=((140-age)*maleabw)/(72*scr)} {else} FOR FEMALE {originalresult=((((140-age)*kg)/(72*scr))*0.85)} {ibwresult=((((140-age)*femaleibw)/(72*scr))*0.85)} {adjustedresult=((((140-age)*femaleabw)/(72*scr))*0.85)} {endif}{endnote}
HEART Score for Cardiac Events
Use this snippet to quickly evaluate the risk of a major adverse cardiovascular event (MACE) in a patient. Quickly complete the standard HEART Score evaluation, and a risk score is returned.
EKG: {formmenu: default=Normal; Non-specific repolarization disturbance; Significant ST deviation; name=EKG} 1 point: No ST deviation but LBBB, LVH, repolarization changes (e.g. digoxin); 2 points: ST deviation not due to LBBB, LVH, or digoxin.
Age: {formmenu: default=<45; 45-64; >65; name=age}
Risk Factors: {formmenu: default=No known risk factors; 1-2 risk factors; >3 risk factors or history of atherosclerotic disease; name=riskfactors} HTN, hypercholesterolemia, DM, obesity (BMI >30 kg/m²), smoking (current, or smoking cessation ≤3 mo), positive family history (parent or sibling with CVD before age 65); atherosclerotic disease: prior MI, PCI/CABG, CVA/TIA, or peripheral arterial disease.
Initial troponin: {formmenu: default=<normal limit; 1-3x normal limit; >3x normal limit; name=troponin} Use local, regular sensitivity troponin assays and corresponding cutoffs
{=score} points {if: score<4}Low Score (0-3 points)
Risk of MACE of 0.9-1.7%.{elseif: score<7}Moderate Score (4-6 points)
Risk of MACE of 12-16.6%.
If troponin is positive, many experts recommend further workup and admission even with a low HEART Score.{elseif: score>6}High Score (7-10 points)
Risk of MACE of 50-65%.{endif}
{if: history="Moderately suspicious"; trim=yes}{q1=1}{elseif: history="Highly suspicious"}{q1=2}{else}{q1=0}{endif}{if: EKG="Non-specific repolarization disturbance"}{q2=1}{elseif: EKG="Significant ST deviation"}{q2=2}{else}{q2=0}{endif}{if: age="45-64"}{q3=1}{elseif: age=">65"}{q3=2}{else}{q3=0}{endif}{if: riskfactors="1-2 risk factors"}{q4=1}{elseif: riskfactors=">3 risk factors or history of atherosclerotic disease"}{q4=2}{else}{q4=0}{endif}{if: troponin="1-3x normal limit"}{q5=1}{elseif: troponin=">3x normal limit"}{q5=2}{else}{q5=0}{endif}{score=q1+q2+q3+q4+q5; trim=yes}
STOP-BANG Assessment
This STOP-BANG calculator was built by a Text Blaze customer who is a physician, who gave permission to share it.
Quickly calculate a STOP-BANG score using this snippet for an assessment, determining risk for obstructive sleep apnea.
| Inputs | Inputs |
|---|---|
| Age: {formmenu: default=≤50 years; >50 years; name=age} | BMI: {formmenu: default=≤35 kg/m²; >35 kg/m²; name=BMI} |
| Neck circumference: {formmenu: default=≤40 cm; >40 cm; name=neck; trim=no} | Gender: {formmenu: default=Female; Male; name=gender; trim=no} |
| Do you snore loudly?: {formmenu: Yes; default=No; name=snore; trim=no} | Daytime Fatigue?: {formmenu: Yes; default=No; name=fatigue; trim=no} |
| During sleep -cessation of breathing has been observed?: {formmenu: Yes; default=No; name=stop; trim=no} | Hx of HTN?: {formmenu: Yes; default=No; name=HTN; trim=no} |
{if: BMI=">35 kg/m²"; trim=yes}{a1=1}{else}{a1=0}{endif} {if: age=">50 years"; trim=yes}{a2=1}{else}{a2=0}{endif} {if: neck=">40 cm"; trim=yes}{a3=1}{else}{a3=0}{endif} {if: gender="Female"; trim=yes}{a4=0}{else}{a4=1}{endif} {if: snore="Yes"; trim=yes}{a5=1}{else}{a5=0}{endif} {if: fatigue="Yes"; trim=yes}{a6=1}{else}{a6=0}{endif} {if: stop="Yes"; trim=yes}{a7=1}{else}{a7=0}{endif} {if: htn="Yes"; trim=yes}{a8=1}{else}{a8=0}{endif} Calculated STOP BANG: {=sum([a1, a2, a3, a4, a5, a6, a7, a8])} -----> {if: sum([a1, a2, a3, a4, a5, a6, a7, a8]) <= 2}Low risk for moderate to severe OSA. {elseif: sum([a1, a2, a3, a4, a5, a6, a7, a8]) <= 4}Intermediate risk for moderate to severe OSA {else} High risk for moderate to severe OSA.{endif}
Ottawa Knee Analysis
The Ottawa Knee rules have been defined as:
a valuable tool for clinicians in the routine management of acute knee injuries. Studies show that they are highly sensitive at identifying patients with fractures of the knee and have a high degree of interobserver agreement and reproducible results.
PECARN Pediatric Head Injury Algorithm
This dot phrase template can be used to complete a PECARN evaluation quickly. This follows the logical order of the assessment, resulting in a recommendation based on the provided answers.
RESULTS {if: age="<2 years" AND q1="no" AND q2="no"}PECARN recommends No CT; Risk of ciTBI <0.02%, “Exceedingly Low, generally lower than risk of CT-induced malignancies.”
{elseif: age="<2 years" AND q1="no" AND q2="yes"}PECARN recommends observation over imaging, depending on provider comfort; 0.9% risk of clinically important Traumatic Brain Injury.
Consider the following when making imaging decisions: Physician experience, worsening signs/symptoms during observation period, age <3 months, parent preference, multiple vs. isolated findings: patients with certain isolated findings (i.e., no other findings suggestive of TBI), such as isolated LOC, isolated headache, isolated vomiting, and certain types of isolated scalp hematomas in infants >3 months have ciTBI risk substantially <1%.
{elseif: age="<2 years" AND q1="yes"}PECARN recommends CT; 4.4% risk of clinically important Traumatic Brain Injury.
{elseif: age=">=2 years" AND q3="yes"}PECARN recommends CT; 4.3% risk of clinically important Traumatic Brain Injury.
{elseif: age=">=2 years" AND q3="no" AND q4="no"}PECARN recommends No CT; Risk <0.05%, “Exceedingly Low, generally lower than risk of CT-induced malignancies.”
{elseif: age=">=2 years" AND q3="no" AND q4="yes"}PECARN recommends observation over imaging, depending on provider comfort; 0.9% risk of clinically important Traumatic Brain Injury.
Consider the following when making imaging decisions: Physician experience, worsening signs/symptoms during observation period, age <3 months, parent preference, multiple vs. isolated findings: patients with certain isolated findings (i.e., no other findings suggestive of TBI), such as isolated LOC, isolated headache, isolated vomiting, and certain types of isolated scalp hematomas in infants >3 months have ciTBI risk substantially <1%.{endif}
CHA2DS2-VASc Calculator and Assessment
The CHA2DS2-VASc score is a clinical prediction rule for estimating the risk of stroke in people with non-rheumatic atrial fibrillation (AF), a common and serious heart arrhythmia associated with thromboembolic stroke.
{note: trim=yes}
CHF history? {formmenu: Yes; default=No; name=CHF; cols=6}
Hypertension history? {formmenu: Yes; default=No; name=hypertension; cols=6}
Age? {formmenu: default=<65; 65-74; >75; name=age; cols=8}
Diabetes mellitus history? {formmenu: Yes; default=No; name=diabetes; cols=6}
Stroke or TIA symptoms previously? {formmenu: Yes; default=No; name=stroketia; cols=6}
Vascular disease history? {formmenu: default=No; Yes; name=vascular}
(prior MI, peripheral artery disease, or aortic plaque)
Sex: {formmenu: default=; Female; Male; name=sex}
{endnote: trim=left}
CHA₂DS₂-VASc Score: {=chads2}
{if: chads2=0}Stroke risk was 0.2% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 0.3% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=1}Stroke risk was 0.6% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 0.9% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=2}Stroke risk was 2.2% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 2.9% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=3}Stroke risk was 3.2% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 4.6% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=4}Stroke risk was 4.8% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 6.7% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=5}Stroke risk was 7.2% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 10.0% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=6}Stroke risk was 9.7% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 13.6% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=7}Stroke risk was 11.2% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 15.7% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=8}Stroke risk was 10.8% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 15.2% risk of stroke/TIA/systemic embolism.
We realize that 8 points showed a lower risk than 7 points, these were the findings in the study, obviously one should assume all scores ≥7 have a risk >10%.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.
{elseif: chads2=9}Stroke risk was 12.2% per year in >90,000 patients (the Swedish Atrial Fibrillation Cohort Study) and 17.4% risk of stroke/TIA/systemic embolism.
One recommendation suggests a 0 score for men or 1 score for women (no clinical risk factors) is “low” risk and may not require anticoagulation; a 1 score for men or 2 score for women is “low-moderate” risk and should consider antiplatelet or anticoagulation; and a score ≥2 for men or ≥3 for women is “moderate-high” risk and should otherwise be an anticoagulation candidate.{endif}
{note: preview=no; trim=left}
Calculating score based on answers:
CHF: {if: CHF="Yes"}{chfscore=1}{else}{chfscore=0}{endif}
Hypertension: {if: hypertension="Yes"}{hypertensionscore=1}{else}{hypertensionscore=0}{endif}
Age: {if: age="65-74"}{agescore=1}{elseif: age=">75"}{agescore=2}{else}{agescore=0}{endif}
Diabetes: {if: diabetes="Yes"}{diabetesscore=1}{else}{diabetesscore=0}{endif}
Stroke/TIA: {if: stroketia="Yes"}{stroketiascore=2}{else}{stroketiascore=0}{endif}
Vascular: {if: vascular="Yes"}{vascularscore=1}{else}{vascularscore=0}{endif}
Sex: {if: sex="Female"}{sexscore=1}{else}{sexscore=0}{endif}
Calculating final score:{chads2=chfscore+hypertensionscore+agescore+diabetesscore+stroketiascore+vascularscore+sexscore}{endnote}
Expected Due Date and Gestational Age Calculators
This snippet helps you quickly get a gestational age based on the estimated due-date of a fetus. Thanks to our user @doc_krieger for contributing to this post.
The calculation performed is:
- Last Menstrual Period (LMP) = ultrasound date minus the gestational age at the ultrasound.
- The due date (or expected date of delivery, EDD) = LMP plus 280 days.
Snippets for Common Notes
This section has snippets, or dot phrase templates, for some common notes that medical professionals like doctors and nurses may take repetitively.
Each snippet is for a specific kind of note. Customize any of them to your needs by clicking the Copy to Text Blaze button above any of these snippets.
Diabetes and Blood Sugar Notes
Generate a clear, concise note about a patient's diabetes. This snippet uses multiple checkboxes to make it more dynamic and able to handle a wide variety of applications.
Allergy and Prescription Templates
This snippet helps you quickly and accurately record information about patients’ allergies and prescriptions.
Written Prescription with Options
You can use this snippet to quickly prescribe medications to patients while communicating online. It uses the if command, the note command, and the formmenu command.
{note}Prescribe Ciprofloxacin type:{formmenu: default=Pills; Eye drops; Cipro-only ear drops; Cipro-Steroid ear drops; name=condition}
{endnote: trim=right}
{if: condition="Pills"; trim=yes} Ciprofloxacin (Cipro) {formmenu: 250; default=500; multiple=no} mg has been electronically prescribed. Take one tablet every 12 hours (twice daily) for {formmenu: default=3; 5; 7} days
{elseif: condition="Eye drops"; trim=yes} Ciprofloxacin 0.3% eye drops has been electronically prescribed for conjunctivitis (bacterial eye infection) Place 1 to 2 drops into the eyes 4 times daily for 5 to 7 days
{elseif: condition="Cipro-only ear drops"; trim=yes} Ciprofloxcin ear drops have been electronically prescribed for otitis externa (ear canal infection) Instill contents of 1 single-dose container into affected ear twice daily for 7 days
{elseif: condition="Cipro-Steroid ear drops"; trim=yes} Ciprodex (antibiotic + steroid) ear drops have been electronically prescribed for otitis externa (ear canal infection) Instill 4 drops into affected ear(s) twice daily for 7 days{endif: trim=yes}
Eye and Vision Care Notes
A snippet that creates a customized note about potential eye and vision problems.
UTI Treatment Plan
This snippet can be used to ask a patient about previous care and treatment. It uses the formmenu command, the note command, formulas, and the cursor command.
Uncategorized Snippets
These are other snippets that may be helpful as a medical professional. There's no limit to what Text Blaze can do to improve your efficiency with text entry, note taking, and interacting with your EMR.
If you want to showcase how you use Text Blaze, head to the healthcare section of our community and share your creations!
Back Pain Question List
Displays a series of questions for evaluating patients with back pain based on different personas. Easily know what questions to ask at any time.
{note}Back Pain Red Flags:{formmenu: default=1. Location and history; 2. Numbness or weakness; 3. Incontinence; 4. IVDA; 5. F/C; 6. Immunesuppression; 7. Female < 50 yo CA / wgt loss; 7. Female > 50 yo CA / wgt loss; 7. Male < 50 yo CA / wgt loss; 7. Male > 50 yo CA / wgt loss; 8. Sleep at night; 9. Worsen/alleviateion triggers; 10. What have you tired; 11. What has helped in the past; name=condition}
{endnote: trim=right}
{if: condition="1. Location and history"; trim=yes} I see you have back pain What part of the back -- lower or upper (please be precise)? When did this start? Any fall or trauma? Any heavy lifting? Have you had similar pain before?
{elseif: condition="2. Numbness or weakness"; trim=yes} Any numbness or tingling of either leg or foot? Any weakness of either leg or foot?
{elseif: condition="3. Incontinence"; trim=yes} Any incontinence of urine or stool?
{elseif: condition="4. IVDA"; trim=yes} Pardon the personal question but do you self-inject drugs? I ask because that can put you at risk of a spine infection which is an emergency
{elseif: condition="5. F/C"; trim=yes} Any fever or chills?
{elseif: condition="6. Immunesuppression"; trim=yes} Any possibility of immune-suppression? Do you take steroids? Do you take immune-suppressing drugs? Do you have an risk of HIV?
{elseif: condition="7. Female < 50 yo CA / wgt loss"; trim=yes} Have you ever been diagnosed with cancer? Have you been losing weight unexpectedly Are you up to date on cancer screenings: PAP smear?
{elseif: condition="7. Female > 50 yo CA / wgt loss"; trim=yes} Have you ever been diagnosed with cancer? Have you been losing weight unexpectedly Are you up to date on cancer screenings: colonoscopy, mammogram, PAP smear?
{elseif: condition="7. Male < 50 yo CA / wgt loss"; trim=yes} Have you ever been diagnosed with cancer? Have you been losing weight unexpectedly
{elseif: condition="7. Male > 50 yo CA / wgt loss"; trim=yes} Have you ever been diagnosed with cancer? Have you been losing weight unexpectedly Are you up to date on cancer screenings: colonoscopy and prostate exam?
{elseif: condition="8. Sleep at night"; trim=yes} When is the back pain at its worst? In the morning? At the end of the day? Can you sleep at night?
{elseif: condition="9. Worsen/alleviateion triggers"; trim=yes} What makes the back pain worse? What makes it better?
{elseif: condition="10. What have you tired"; trim=yes} What have you done or taken to alleviate the back pain?
{elseif: condition="11. What has helped in the past"; trim=yes} Have you had similar back pain in the past? What worked to alleviate the pain?{endif: trim=yes}
Physical Therapy Exam - Wrist Fracture Template
The following snippet was shared with us by a practicing Physical Therapist for their initial examination/evaluation of a patient that has a fractured wrist.
DX/SURGERY: {formtext: name=dxsurgery; default=Right/Left distal radius fracture S/P ORIF; cols=35}
DOS: {formparagraph: name=dos}
PRIMARY COMPLAINTS: {formparagraph: name=primarycomplaints; cols=35; rows=4}
PRIOR FUNCTIONAL STATUS: {formparagraph: name=priorstatus; cols=35; rows=4}
CURRENT FUNCTIONAL STATUS: See "Client Information Sheet" for activities that patient reports having difficulty with. Client reports difficulty in the following activities: {formmenu: name=activities; values=eating/using utensils, drinking, bathing/showering, dressing, grooming/toileting, cooking/meal preparation, opening jars & bottles, opening medication, lifting pots & pans, lifting bags & groceries, house cleaning, driving, using keys, writing, keyboarding/mouse use, texting/holding phone, weight-bearing through hand/wrist, gardening/yard work, and hobbies; multiple=yes}
Occupation: {formtext: name=occupation} Social Status: {formtext: name=social status}
PAIN: Pain location: {formtext: name=painlocation} At worst: {formmenu: name=worstpain; values={=seq(1,10)}}/10 Current: {formmenu: name=currentpain; values={=seq(1,10)}}/10 At best: {formmenu: name=bestpain; values={=seq(1,10)}}/10 Pain description: {formtext: name=paindescription} Pain Follow-up Plan: {formparagraph: name=followupplan; cols=35; rows=4}
PATIENT GOALS: {formparagraph: name=patientgoals; cols=35; rows=4}
OBJECTIVE FINDINGS: Handedness: {formmenu: default=Right; Left; Ambidextrous; name=handedness} Wound / Incision Status: {formparagraph: name=woundstatus; cols=35; rows=4} Orthosis/Splint Use: {formparagraph: name=splintuse; cols=35; rows=4} Swelling: {formparagraph: name=swelling; cols=35; rows=4}
Circumferential measurements (cms): Right MCPs: {formtext: name=rightmcps; cols=2}cm Left MCPs: {formtext: name=leftmcps; cols=2}cm Right Wrist: {formtext: name=rightwrist; cols=2}cm Left Wrist: {formtext: name=leftwrist; cols=2}cm
Right Left Digit AROM (extension is 0 unless otherwise indicated): {formparagraph: name=arom; cols=35; rows=4}
Thumb AROM: IP: left: {formtext: name=leftthumbIP} || right: {formtext: name=rightthumbIP} MP: left: {formtext: name=leftthumbMP} || right: {formtext: name=rightthumbIP} Plan abd: left: {formtext: name=leftthumbPlanabd} || right: {formtext: name=rightthumbPlanabd} Palm abd: left: {formtext: name=leftthumbPalmabd} || right: {formtext: name=rightthumbPalmbabd} Opp: left: {formtext: name=leftthumbOpp}|| right: {formtext: name=rightthumbOpp}
Wrist AROM: E: left: {formtext: name=leftwristaromE} || right: {formtext: name=rightwristaromE} F: left: {formtext: name=leftwristaromF} || right: {formtext: name=rightwristaromF} RD: left: {formtext: name=leftwristaromRD} || right: {formtext: name=rightwristaromRD} UD: left: {formtext: name=leftwristaromUD} || right: {formtext: name=righttwristaromUD}
Forearm AROM: Sup: left: {formtext: name=leftforearmaromSup}|| right: {formtext: name=rightforearmaromSup} Pron: left: {formtext: name=leftforearmaromPron} || right: {formtext: name=rightforearmaromPron}
Shoulder AROM: WFL: left: {formtext: name=leftshoulderaromWFL} || right: {formtext: name=rightshoulderaromWFL} Flexion: left: {formtext: name=leftshoulderaromFlexion} || right: {formtext: name=rightshoulderaromFlexion} Extension: left: {formtext: name=leftshoulderaromExtension} || right: {formtext: name=rightshoulderaromExtension} Abduction: left: {formtext: name=leftshoulderaromAbduction} || right: {formtext: name=rightshoulderaromAbduction} IR: left: {formtext: name=leftshoulderaromIR} || right: {formtext: name=rightshoulderaromIR} ER: left: {formtext: name=leftshoulderaromER} || right: {formtext: name=rightshoulderaromER}
Grip and Pinch Strength: {formparagraph: name=grippinch; cols=35; rows=4}
Sensation: {formparagraph: name=sensation; cols=35; rows=4}
Palpation: {formparagraph: name=Palpation; cols=35; rows=4}
MODERATE COMPLEXITY OT CODE: The patient's occupational profile and medical and therapy histories were reviewed through {formtext: name=historyreviewed; cols=35}, and patient intake forms. An analysis was completed of the occupational profile/data based on a detailed assessment. The evaluation identified {formtext: name=resultsidentified; cols=35}. Clinical decision making involved moderate analytic complexity and consideration of several treatment options. Minimal to moderate modification of tasks or assistance was provided. COVID19 precautions in effect.
Generate a List of Symptoms
This snippet focuses on eye-related symptoms. It's easily customized by clicking "Copy to Text Blaze" to add it to your account, and then changing the available options in the menu inside the snippet.
How to Create and Edit Snippets Yourself
These snippets include dynamic commands. If you’re interested in learning how to create these yourself, visit the pages below to learn more.
- Time
- Forms (to turn your snippets into customizable templates) (Pro, Business, and Enterprise Plans)
- Formulas (Pro, Business, and Enterprise Plans)
- Logic (if/ then) (Pro, Business, and Enterprise Plans)
Once you get comfortable with these features, head to your dashboard and give it a try yourself!
You can also copy these snippets directly into your dashboard and customize them to fit your needs.